As a resurgence of Covid-19 continues to put pressure on the healthcare system in the Australian state of Victoria, elective surgery remains suspended until further notice. But while retaining capacity to deal with the new outbreak is crucial, the cancellation of surgery and the resulting backlog could have severe consequences for patients waiting for procedures.
The state government had initially planned to give all Victorian hospitals the green light to return to 100% of their usual elective surgery operating theatre capacity in July in line with other Australian states and territories. However, in recent weeks thousands of new Covid-19 cases have been recorded in an outbreak described as a second wave.
In its initial response to the rise in cases, the state government advised hospitals to keep surgical activity at 75% of pre-pandemic levels to ensure there was sufficient capacity to treat Covid-19 patients. This was followed in July by a ban on non-urgent elective surgery in Melbourne, where the majority of cases have been identified, in response to further rises.
More recently, it has become clear that the government is dealing with a major outbreak, prompting Victorian Premier Daniel Andrews to announce that all surgical activity beyond category one and the most urgent category two would be suspended state wide in public hospitals. The stricter measures were introduced to allow hospitals to remain prepared for further rises in Covid-19 patient numbers and focus on lifesaving care, and will be in place until further notice.
As a result, the state’s plan to catch up on its expanding hospital waiting list has been put on hold, meaning patients waiting for elective surgery in Victoria’s public hospitals will face even longer waiting times. It is thought the effect will be felt particularly among those waiting for orthopaedic and ophthalmic surgery, since many procedures in these areas are elective and waiting times were already relatively high. The potential impact on patients include a worsening of conditions, extended pain and suffering, reduced mobility and discomfort.
Analysis by The Sydney Morning Herald and The Age in July estimates that around 120,000 people will have been added to public hospital waiting lists during the shutdown period, including about 36,000 in Victoria (a 71% increase) and about 32,400 in NSW (a 36% increase). An earlier global study estimated that around 400,000 elective procedures may already have been cancelled in Australia during the ongoing pandemic.
Public hospitals in Australia were already overstretched before the arrival of COVID-19, with the number of people added to waiting lists for elective surgery each year outstripping the number of operations performed.
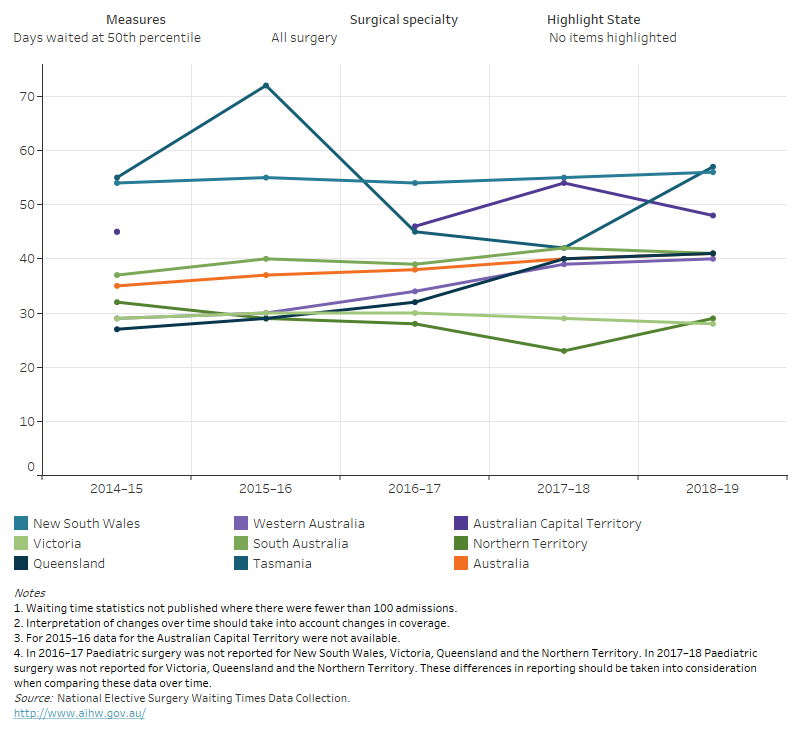
According to the latest national figures from the Australian Institute of Health and Welfare, which are for 2018-19, 890,000 patients were added to public hospital elective surgery waiting lists nationally during 2018-19, while only 760,000 people were admitted for surgery. 50% of all patients waited at least 41 days for admission in 2018-19, up from a median waiting time of 35 days only five years earlier.
 The latest set of figures for Victoria, which cover the period up to June 2020, show that – unsurprisingly – elective surgery activity has fallen substantially compared to last year, while the waiting list has increased.
The latest set of figures for Victoria, which cover the period up to June 2020, show that – unsurprisingly – elective surgery activity has fallen substantially compared to last year, while the waiting list has increased.
In June, there were just over 56,000 patients on the elective surgery waiting list.
What’s more, waiting lists are likely to continue to grow over the foreseeable future.
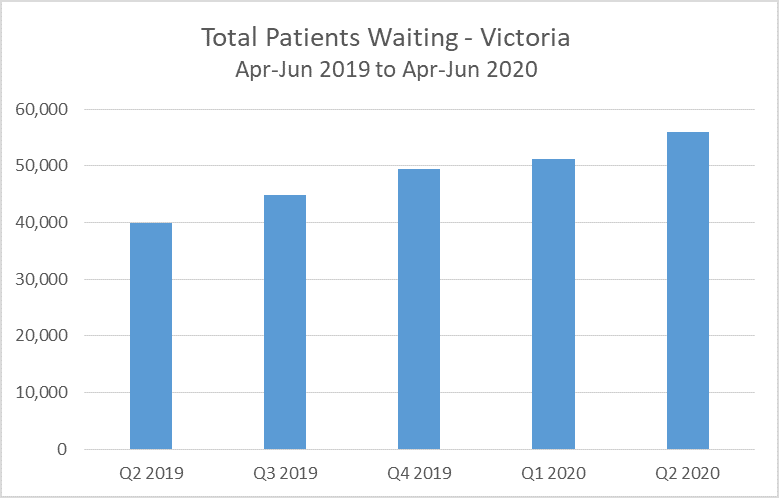 These figures do not include missing referrals from primary care – those who put off seeking care during Covid-19.
These figures do not include missing referrals from primary care – those who put off seeking care during Covid-19.
And even when elective surgery is restarted, theatre throughput will be reduced as a result of the additional precautions required to ensure the safety of both patients and staff, and it is unlikely 100% of pre-Covid capacity will be reached immediately following a resumption.
Government guidance on restarting surgery outlines a phased approach to restarting surgery, although it us up to each State/Territory to determine which stage applies to its circumstances. These stages are:
- Stage 1 – up to 50 per cent of normal surgical activity levels;
- Stage 2 – up to 75 per cent of normal surgical activity levels;
- Stage 3 – up to 100 per cent of normal surgical activity levels or as close to normal activity levels as is safely possible.
While some surgery has been able to continue, such as urgent and critical cases as well as some elective cases within the private sector, additional capacity will likely be needed to support public hospitals’ efforts. One way to quickly add significant capacity and protect elective surgery capacity during the pandemic is to use flexible healthcare solutions. .
A mobile or modular operating theatre, combined with a ward for patients recovering from procedures, can provide a complete, stand-alone ‘cold’ or ‘clean’ site for treating patients safely during the pandemic and prevent waiting lists from growing, while maintaining crucial Covid-19 capacity within the hospital building.
By default, mobile theatres offer separate entrance and exit routes, as well as anaesthetic, treatment and recovery rooms, and can also be configured to include a dedicated reception area, waiting room, staff rest areas and changing rooms. An additional benefit of using a stand-alone facility is that it provides extra reassurance for patients who may be concerned about going to hospital and have put off or cancelled appointments for fear of contracting Covid-19.
Waiting lists for elective surgery are expected to remain inflated for some time, leading to longer waiting times and potentially serious consequences for patients, and a ‘hidden’ backlog of patients caused by delayed referrals is also widely expected to add to elective surgery waiting list in the coming months. It’s clear that more capacity will be needed to catch up. The previously mentioned global study on cancelled surgery estimated that, even at 120% of pre-Covid capacity, it would take 22 weeks to clear the backlog.
Once surgery within hospitals start to scale up, the use of a mobile or modular theatre at the hospital site can be used together with the hospital’s internal theatre capacity, to enable earlier resumption of activity at levels up to 100% of pre-Covid capacity, or potentially even above 100%, allowing hospitals to reduce waiting lists quickly.






